Can a single stroke destroy your memory and thinking abilities forever?
This question haunts millions of stroke survivors and their families who notice changes in cognitive function after a stroke event.
The answer is both complex and concerning: yes, strokes can directly cause dementia, and the risk increases significantly with each stroke episode.
Understanding the connection between strokes and dementia helps families recognize warning signs, seek appropriate treatment, and take steps to prevent further cognitive decline.
What Is Vascular Dementia?
Vascular dementia represents the second most common type of dementia after Alzheimer’s disease, accounting for approximately 20% of all dementia cases worldwide.
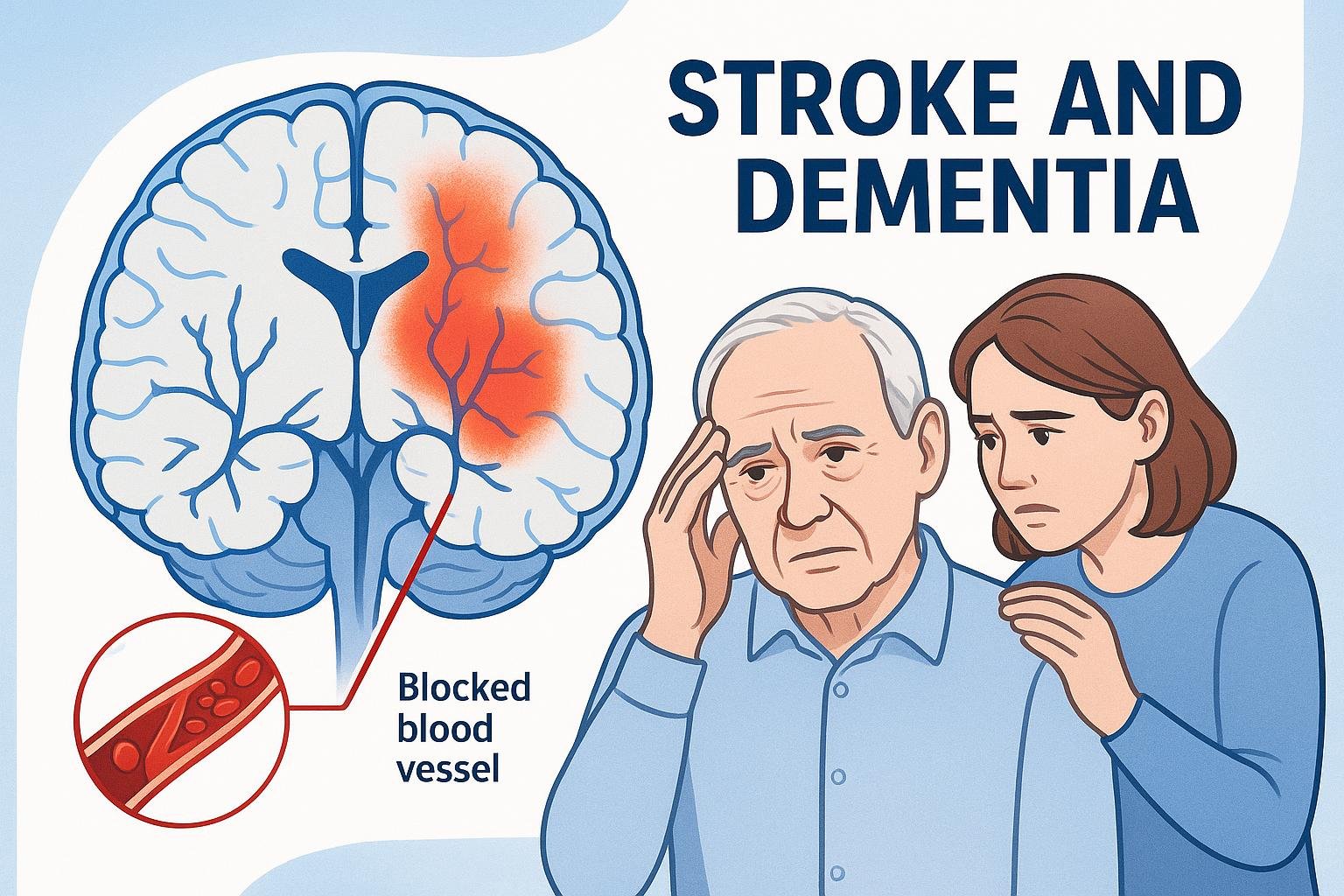
How Strokes Cause Dementia
Strokes damage brain tissue by cutting off blood supply to specific brain regions:
•Direct brain damage: Stroke destroys brain cells in memory, language, and thinking areas
•Reduced blood flow: Multiple small strokes accumulate damage over time, starving brain tissue of oxygen
•Inflammatory responses: Stroke triggers brain inflammation that accelerates cognitive decline
Types of Stroke-Related Cognitive Problems
Post-stroke cognitive impairment: Mild thinking problems that may improve with rehabilitation and don’t always progress to dementia.
Vascular dementia: Severe cognitive decline affecting daily life, with multiple brain functions impaired and symptoms interfering with independence.
Mixed dementia: Combination of vascular and Alzheimer’s changes, requiring comprehensive treatment approaches.
Risk Factors and Prevention

Understanding risk factors helps families take proactive steps to prevent stroke-related dementia.
Major Risk Factors
Medical conditions:
•High blood pressure (most significant risk factor)
•Multiple strokes dramatically increase dementia risk
•Diabetes affects blood vessel health
•Heart disease reduces blood flow to the brain
•High cholesterol contributes to artery blockages
Stroke characteristics:
•Location and size of brain damage
•Silent strokes causing gradual cognitive decline
•Age over 65 significantly increases risk
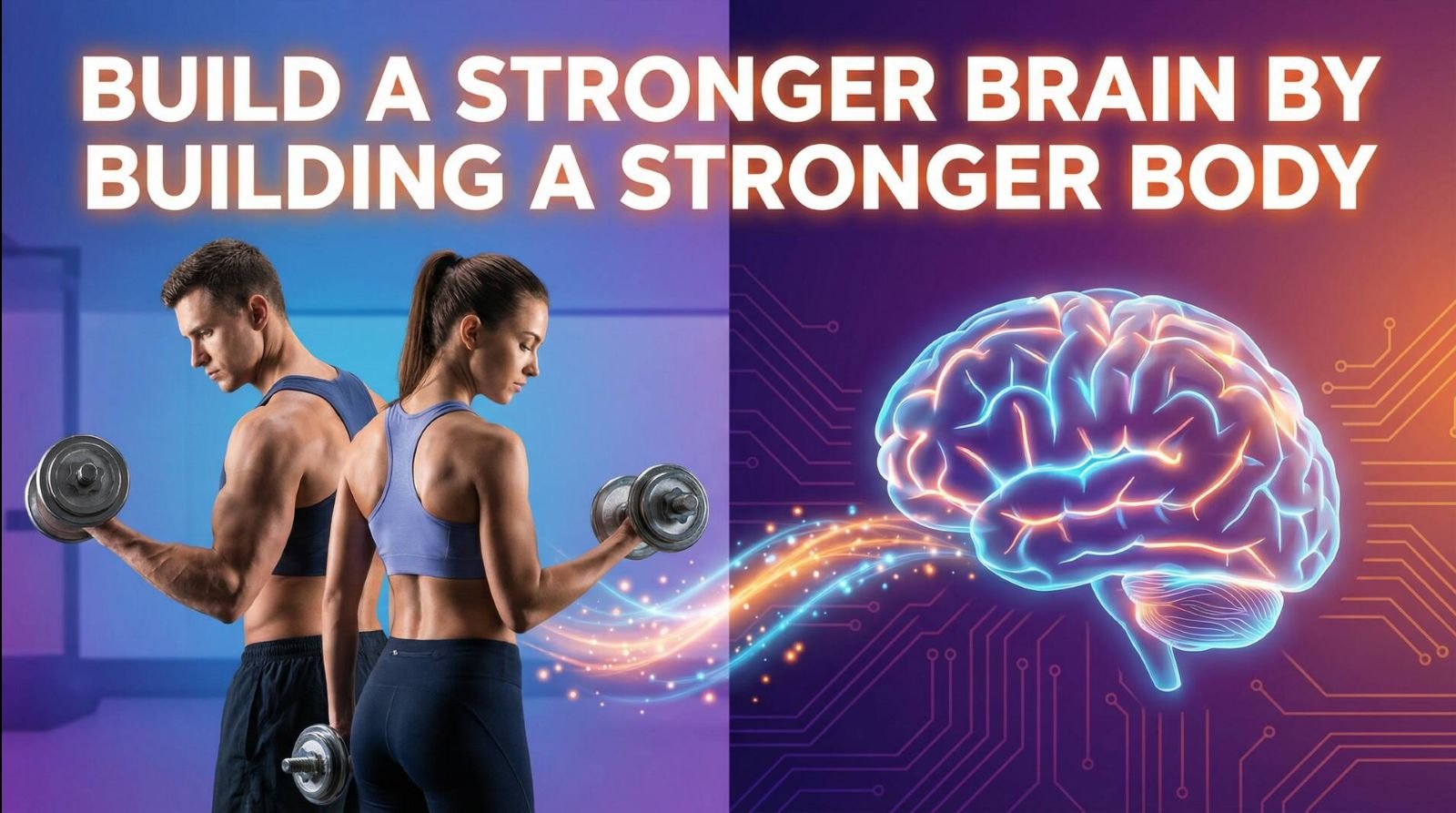
Lifestyle factors:
•Smoking damages blood vessels throughout the body
•Physical inactivity reduces circulation
•Excessive alcohol consumption affects brain health
•Poor diet contributes to cardiovascular problems
| Risk Factor | Impact Level | Modifiable | Prevention Strategy |
| High blood pressure | Very High | Yes | Medication, diet, exercise |
| Multiple strokes | Very High | Partially | Stroke prevention measures |
| Diabetes | High | Yes | Blood sugar control |
| Smoking | High | Yes | Smoking cessation programs |
| Age over 75 | High | No | Focus on other risk factors |
Prevention Strategies

Primary prevention (before first stroke):
•Control blood pressure through medication and lifestyle changes
•Manage diabetes with proper diet, exercise, and medication
•Quit smoking and limit alcohol consumption
•Regular exercise improves circulation and supports brain health
•Mediterranean-style diet protects blood vessels
•Maintain healthy weight and get adequate sleep
Secondary prevention (after stroke):
•Take prescribed medications consistently
•Attend all follow-up medical appointments
•Monitor for signs of additional strokes
•Participate in rehabilitation programs
Recognizing Symptoms
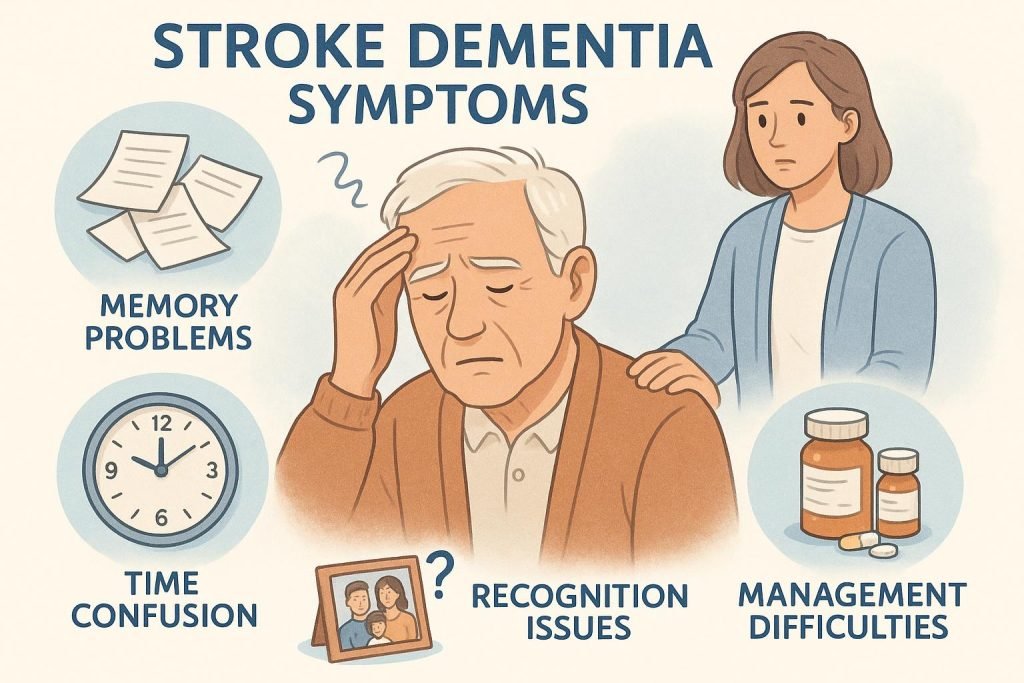
Stroke-related dementia symptoms can appear immediately after a stroke or develop gradually over time.
Immediate Post-Stroke Changes
Cognitive symptoms:
•Sudden confusion or disorientation
•Difficulty understanding instructions
•Problems with memory formation
•Trouble recognizing familiar people or places
Communication problems:
•Difficulty finding words or speaking clearly
•Problems understanding spoken language
•Reading and writing abilities affected
Executive function issues:
•Difficulty making decisions or solving problems
•Poor judgment in daily situations
•Trouble planning or organizing activities
Progressive Symptoms
Memory and daily living:
•Forgetting recent events or conversations
•Difficulty learning new information
•Problems managing medications or finances
•Getting lost in familiar places
Behavioral changes:
•Increased irritability or mood swings
•Depression or anxiety following stroke
•Personality changes or inappropriate behavior
•Reduced motivation or interest in activities
Diagnosis and Medical Evaluation
Comprehensive medical assessment distinguishes stroke-related dementia from other types of cognitive decline.
Medical evaluation includes:
•Documentation of all previous strokes or mini-strokes
•Timeline of cognitive changes relative to stroke events
•Standardized cognitive tests measuring memory, thinking, and language
•Brain imaging (CT/MRI scans) to identify stroke damage
•Blood work to rule out other medical conditions
Specialized testing:
•PET scans show brain metabolism patterns
•Advanced MRI techniques detect small vessel disease
•Serial imaging tracks changes over time
Treatment and Management
While stroke-related dementia cannot be cured, treatments can slow progression and improve quality of life.
Medical Treatments
Stroke prevention medications:
•Blood thinners reduce risk of future strokes
•Blood pressure medications protect blood vessels
•Cholesterol-lowering drugs improve circulation
•Diabetes medications control blood sugar levels
Cognitive enhancement:
•Some Alzheimer’s medications may help vascular dementia
•Cholinesterase inhibitors can improve thinking abilities
•Memantine may help with moderate to severe symptoms
Rehabilitation and Support
Therapeutic interventions:
•Speech therapy for language and communication problems
•Occupational therapy maintains daily living skills
•Physical therapy improves mobility and reduces fall risk
•Cognitive training exercises may help specific abilities
Family support:
•Understanding stroke-related dementia helps families cope
•Learning communication strategies improves interactions
•Safety planning prevents accidents and injuries
•Respite care provides breaks for family caregivers
Living with Stroke-Related Dementia
Daily Management Strategies
Communication techniques:
•Speak slowly and clearly using simple sentences
•Allow extra time for responses
•Use visual cues and gestures when helpful
Safety and independence:
•Remove tripping hazards and improve lighting
•Install grab bars and safety equipment
•Use memory aids and organizational tools
•Establish consistent daily routines
Support Resources
Healthcare team:
•Neurologist specializes in brain and stroke care
•Geriatrician focuses on aging-related health issues
•Social worker helps coordinate care and resources
•Therapists provide ongoing rehabilitation services
Community support:
•Stroke support groups connect families with similar experiences
•Adult day programs provide social interaction and supervision
•Respite care services give family caregivers breaks
Prognosis and Recovery Potential
The outlook varies significantly based on stroke characteristics, individual factors, and access to quality care.
Factors affecting prognosis:
•Location and size of brain damage
•Number of strokes experienced
•Age at time of stroke and diagnosis
•Overall health and cognitive reserve
Recovery expectations:
•Some cognitive abilities may improve with rehabilitation and medications
•Complete recovery of lost abilities is rare
•Focus on maintaining remaining abilities and independence
•Early intervention provides the best outcomes
Research and Future Directions
Scientists continue developing better treatments and prevention strategies:
Current research:
•New medications to protect brain cells after stroke
•Therapies to improve blood flow to damaged brain areas
•Stem cell research for brain repair and regeneration
•Better brain imaging to detect early changes
Promising developments:
•Telemedicine for remote monitoring and care
•Cognitive training apps and computer programs
•Genetic testing to identify high-risk individuals
•Personalized medicine approaches for stroke prevention
Key Takeaways
Yes, strokes can cause dementia, particularly vascular dementia resulting from brain damage due to reduced blood flow. The risk increases with multiple strokes, advanced age, and poor cardiovascular health management.
Prevention remains the most effective strategy – controlling blood pressure, managing diabetes, maintaining heart health, and adopting brain-healthy lifestyle habits significantly reduce risk.
Early recognition of stroke-related cognitive changes allows for prompt medical intervention that may slow progression. While complete recovery is rare, rehabilitation, medications, and lifestyle changes help maintain cognitive abilities and quality of life.
Understanding this connection empowers families to take proactive prevention steps, seek appropriate treatment, and plan for long-term care needs. With proper support, people with stroke-related cognitive changes can continue living meaningful lives with dignity and independence.
Frequently Asked Questions
Q: How quickly can dementia develop after a stroke?
A: Cognitive changes can appear immediately or develop gradually over months to years.
Q: Can stroke-related dementia be reversed?
A: While brain damage cannot be completely reversed, some abilities may improve with rehabilitation, medications, and lifestyle changes.
Q: What’s the difference between stroke-related dementia and Alzheimer’s?
A: Stroke-related dementia results from blood flow problems, while Alzheimer’s involves protein deposits. Stroke-related dementia often has more sudden onset.
Q: How can I reduce my risk?
A: Focus on cardiovascular health: control blood pressure, manage diabetes, quit smoking, exercise regularly, and eat a heart-healthy diet.
Q: Is it hereditary?
A: While not directly inherited, genetic factors that increase stroke risk can run in families.