Does your loved one with dementia accuse you of stealing their belongings? Do they believe that family members are trying to harm them or that strangers are in their home? Are you struggling to understand why someone who once trusted you completely now views you with suspicion? These experiences are heartbreaking for families but represent common symptoms of dementia.
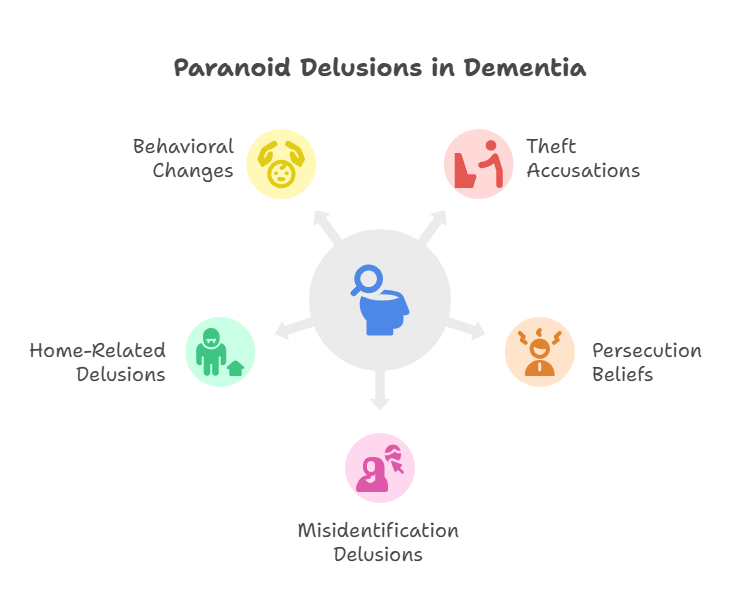
Paranoia and delusions are frequent symptoms in dementia patients, affecting their perception of reality and relationships with loved ones. These strongly held false beliefs can take various forms, from accusations of theft to beliefs that family members are impostors trying to cause harm.
Understanding that delusions feel completely real to dementia patients helps families respond more effectively and maintain emotional connections despite these challenging behaviors. The paranoid thoughts and accusations stem from brain changes rather than actual events, but they create genuine distress for both patients and their caregivers.
Understanding Paranoia and Delusions in Dementia
Delusions represent strongly held false beliefs that are not based on reality or evidence. In dementia patients, these beliefs often take the form of paranoia, making patients feel threatened even when there is no reasonable basis for such feelings. The brain changes associated with dementia can make patients suspicious of the people around them, including their closest family members.
Paranoid delusions in dementia differ significantly from temporary suspicions or concerns that healthy individuals might experience. These beliefs persist despite evidence to the contrary and often become more elaborate over time. Patients experiencing delusions may feel they are being watched, that someone is acting against them, or that people are plotting to harm them.
The inability to process information correctly represents a key factor in the development of delusions. Dementia patients may be unable to put bits of information and memories together accurately, leading them to draw false conclusions and believe things that are not true. This cognitive impairment affects their ability to evaluate situations rationally.
Delusions become more likely as dementia progresses and worsens over time. The prevalence of delusions varies by dementia type, with dementia with Lewy bodies showing the highest rates of paranoid symptoms. Alzheimer’s disease and vascular dementia patients also experience delusions, particularly in later stages of the disease.
The emotional impact of delusions on patients can be severe. These false beliefs often create negative feelings, fear, and distress. Patients may become frightened, angry, or withdrawn as a result of their paranoid thoughts. Understanding this emotional component helps families respond with greater empathy and effectiveness.
| Delusion Type | Common Examples | Frequency in Dementia | Typical Response Strategy |
|---|---|---|---|
| Theft delusions | Missing items believed stolen | Very common | Help search, avoid arguing |
| Persecution delusions | Belief others want to harm them | Common | Provide reassurance, validate feelings |
| Misidentification | Partner is an impostor | Moderate | Gentle redirection, avoid confrontation |
| Home delusions | This isn’t their real home | Moderate | Acknowledge feelings, distract |
What Research Shows About Paranoia in Dementia
Research from Alzheimer’s Society demonstrates that delusions are common symptoms for people with dementia, often manifesting as paranoia that makes patients feel threatened without reasonable cause [1]. These symptoms represent neurological changes rather than personality flaws or intentional behaviors.
Brain damage patterns explain why delusions develop in dementia patients. The disease affects areas responsible for memory processing, reasoning, and reality testing. When these brain regions cannot function properly, patients may misinterpret normal situations as threatening or dangerous.
Progression patterns show that delusions typically worsen as dementia advances. Early-stage patients may experience occasional suspicious thoughts, while those in later stages may develop elaborate paranoid belief systems. The frequency and intensity of delusions generally increase over time, requiring adapted management strategies.
Type-specific differences in delusion patterns help predict what families might expect. Lewy body dementia patients often experience visual hallucinations alongside paranoid delusions, creating complex symptom presentations. Alzheimer’s disease patients typically develop delusions in middle to later stages, while frontotemporal dementia patients may show different patterns of paranoid thinking.
Research findings indicate that delusions create significant stress for both patients and caregivers. Studies show that families dealing with paranoid behaviors experience higher levels of burden and emotional distress. This creates a challenging cycle where patient symptoms increase family stress, which can inadvertently worsen the patient’s paranoid feelings.
The Neuroscience of Delusions
Brain imaging studies reveal specific patterns of damage associated with delusions in dementia. Areas involved in reality monitoring, memory consolidation, and emotional regulation show particular vulnerability. When these regions cannot communicate effectively, patients may develop false beliefs about their experiences.
Neurotransmitter changes also contribute to delusion development. Alterations in dopamine, acetylcholine, and other brain chemicals can affect perception and interpretation of events. These chemical imbalances may make patients more susceptible to paranoid thoughts and less able to correct false beliefs.
Memory fragmentation plays a crucial role in delusion formation. When patients cannot remember recent events clearly, they may create explanations that seem logical to them but are based on incomplete or inaccurate information. These explanations can evolve into persistent delusions over time.
Signs and Symptoms to Watch For
Recognizing paranoid delusions in dementia patients requires understanding both the content of their beliefs and the behavioral changes that accompany these symptoms. Families should monitor for specific patterns that suggest developing or worsening paranoid thinking.
Theft accusations represent the most common type of delusion in dementia patients. When patients cannot find personal items such as clothing, jewelry, or important documents, they may conclude that someone has stolen these belongings. This belief can persist even when the items are found in unusual places where the patient had hidden them.
Persecution beliefs involve patients thinking that others are trying to harm them in various ways. These may include beliefs that food is being poisoned, that medications are harmful, or that family members are plotting against them. Patients may become suspicious of previously trusted individuals and resist their help or presence.
Misidentification delusions occur when patients believe that familiar people are actually impostors. Capgras syndrome represents a specific type where patients think their spouse or family member has been replaced by an identical-looking stranger. This can be particularly distressing for families who suddenly find themselves viewed as threats.
Home-related delusions involve patients believing that their current residence is not their real home. They may insist on “going home” even when they are in their longtime residence, or claim that strangers are living in their house. These beliefs often relate to time-shifting, where patients think they are living in an earlier period of their lives.
Behavioral changes accompanying delusions include increased agitation, resistance to care, social withdrawal, and aggressive responses to perceived threats. Patients may hide belongings, refuse to eat, or become combative when their delusions are challenged or dismissed.
Early Warning Signs
Subtle changes in trust and suspicion often precede more obvious delusions. Patients may begin questioning the motives of family members, expressing unusual concerns about safety, or showing increased vigilance about their belongings. These early signs provide opportunities for intervention before delusions become firmly established.
Communication patterns may shift as paranoid thinking develops. Patients might ask repeated questions about the whereabouts of items, express concerns about people’s intentions, or make comments that suggest they feel threatened or unsafe. These verbal cues can alert families to developing problems.
Sleep disturbances often accompany paranoid delusions. Patients may have difficulty sleeping due to fears about safety, or they may wake frequently to check on their belongings. These sleep problems can worsen cognitive function and increase susceptibility to delusions.
Causes and Risk Factors
Multiple factors contribute to the development of paranoid delusions in dementia patients. Understanding these causes helps families recognize why delusions occur and what circumstances might trigger or worsen paranoid thinking.
Primary brain changes represent the fundamental cause of delusions in dementia. Damage to areas responsible for memory processing, reality testing, and emotional regulation creates the neurological foundation for paranoid thinking. As these brain regions deteriorate, patients lose the ability to accurately interpret their experiences.
Memory impairment plays a central role in delusion development. When patients cannot remember where they placed items or what happened during recent events, they may create explanations that involve other people taking their belongings or acting against them. These explanations can become fixed beliefs that resist correction.
Sensory impairments can contribute to paranoid thinking by making it difficult for patients to accurately perceive their environment. Vision problems may cause patients to misidentify people or objects, while hearing difficulties can lead to misinterpretation of conversations or sounds. These sensory issues can fuel paranoid beliefs about threats or dangers.
Environmental factors influence the likelihood and severity of delusions. Unfamiliar surroundings, changes in routine, or introduction of new people can trigger paranoid responses in vulnerable patients. Maintaining familiar environments and consistent caregivers helps reduce delusion risk.
| Risk Factor | Impact Level | Prevention Strategy | Management Approach |
|---|---|---|---|
| Memory impairment | High | Cognitive stimulation | Gentle reality orientation |
| Sensory problems | Moderate | Regular vision/hearing checks | Environmental modifications |
| Environmental changes | Moderate | Maintain familiar settings | Gradual transitions |
| Medication effects | Variable | Regular medication reviews | Dosage adjustments |
| Social isolation | Moderate | Maintain social connections | Structured activities |
Medication effects can trigger or worsen delusions in some patients. Certain drugs used to treat other conditions may have side effects that increase paranoid thinking. New medications or changes in dosages should be monitored carefully for their impact on delusion symptoms.
Physical health problems can contribute to delusion development. Infections, pain, dehydration, or other medical conditions can worsen cognitive function and increase susceptibility to paranoid thinking. Addressing these underlying health issues may help reduce delusion severity.
Management and Support Strategies
Supporting patients with delusions requires approaches that prioritize emotional comfort and safety while avoiding confrontation about the false beliefs. The goal is to maintain relationships and reduce distress rather than convince patients that their beliefs are incorrect.
Validation techniques prove most effective for managing paranoid delusions. Rather than arguing with patients about the reality of their beliefs, caregivers should acknowledge their feelings and provide emotional support. Statements like “That must be very frightening for you” validate the patient’s emotional experience without reinforcing the delusion.
Gentle redirection helps move conversations away from paranoid topics without directly challenging the beliefs. When patients express paranoid thoughts, caregivers can acknowledge their concerns and then suggest engaging in a pleasant activity or discussing a different topic. This approach reduces agitation while providing distraction.
Environmental modifications can help prevent situations that trigger paranoid thinking. Consistent placement of important items reduces the likelihood of “theft” accusations. Familiar surroundings and routine schedules help patients feel more secure and less suspicious of their environment.
Communication strategies should emphasize reassurance and emotional connection. Using calm tones, simple language, and non-threatening body language helps patients feel safer. Caregivers should avoid arguing, providing excessive explanations, or becoming defensive when accused of wrongdoing.
Safety considerations become important when delusions involve fears of harm or threats. While maintaining emotional support, caregivers must ensure that paranoid beliefs do not lead to dangerous behaviors such as refusing medications, leaving the home unsupervised, or becoming aggressive toward others.
Practical Response Techniques
When accusations occur, caregivers should remain calm and avoid taking the accusations personally. Responses like “I can see you’re upset about your missing ring. Let’s look for it together” acknowledge the patient’s concern while offering practical help. This approach maintains the relationship while addressing the immediate issue.
Distraction methods can be effective when delusions cause significant distress. Engaging patients in enjoyable activities, playing familiar music, or involving them in simple tasks can redirect their attention away from paranoid thoughts. The key is finding activities that capture their interest and provide positive experiences.
Routine establishment helps create predictability that can reduce paranoid thinking. When patients know what to expect throughout the day, they may feel more secure and less likely to develop suspicious thoughts about changes or unexpected events.
When to Seek Medical Help
Medical evaluation becomes necessary when paranoid delusions significantly impact the patient’s quality of life, safety, or relationships with family members. Healthcare providers can assess the severity of symptoms and recommend appropriate interventions.
Immediate medical attention is required when delusions lead to dangerous behaviors such as refusing to eat due to poisoning fears, attempting to leave home to escape perceived threats, or becoming physically aggressive toward caregivers. These situations require prompt professional intervention.
Medication considerations may be appropriate for severe or persistent delusions that do not respond to behavioral interventions. Antipsychotic medications can sometimes help reduce delusion severity, but they should only be used when other approaches have failed due to potential side effects. These medications require careful monitoring, especially in patients with Lewy body dementia who are at higher risk for adverse reactions.
Regular monitoring helps track delusion patterns and treatment effectiveness. Healthcare providers should assess whether delusions are worsening, remaining stable, or improving with current interventions. This information guides decisions about treatment modifications.
Signs requiring medical evaluation include sudden onset of new delusions, significant increase in paranoid behaviors, delusions that interfere with basic care activities, or development of aggressive behaviors related to paranoid thinking.
| Situation | Urgency Level | Recommended Action |
|---|---|---|
| Dangerous behaviors from delusions | High | Immediate medical evaluation |
| New or worsening delusions | Moderate | Schedule medical appointment |
| Medication-related delusions | High | Contact prescribing physician |
| Delusions interfering with care | Moderate | Discuss with healthcare team |
| Family safety concerns | High | Seek immediate professional help |
Specialist consultations may be beneficial for complex delusion management. Geriatric psychiatrists, neurologists, or geriatricians with dementia expertise can provide specialized assessment and treatment recommendations for challenging cases.
Frequently Asked Questions
Why do dementia patients become paranoid?
Paranoid thinking develops in dementia patients due to brain damage that affects areas responsible for memory, reasoning, and reality testing. When patients cannot process information correctly or remember recent events, they may create explanations involving theft or harm that seem logical to them but are based on incomplete or inaccurate information. This represents a neurological symptom rather than a personality change or intentional behavior.
Should you argue with dementia patients about their delusions?
Arguing with delusions is generally ineffective and often increases patient distress and agitation. Since delusions feel completely real to patients, attempts to convince them otherwise typically fail and can damage the caregiver relationship. Instead, caregivers should validate the patient’s emotions, provide reassurance, and gently redirect conversations to more positive topics.
Can paranoid delusions in dementia be treated?
Treatment approaches for paranoid delusions include both behavioral interventions and, when necessary, medications. Environmental modifications, communication strategies, and routine establishment often help reduce delusion frequency and severity. In severe cases, antipsychotic medications may be considered, but these require careful monitoring due to potential side effects, especially in patients with Lewy body dementia.
How should families respond to theft accusations?
Theft accusations should be handled with patience and understanding. Rather than denying the accusation or becoming defensive, caregivers can acknowledge the patient’s distress and offer to help search for the missing item. Statements like “I can see you’re worried about your wallet. Let’s look for it together” validate feelings while providing practical assistance. Avoiding arguments helps maintain trust and emotional connection.
Do all dementia patients develop paranoid delusions?
Not all dementia patients develop significant paranoid delusions, and the severity varies considerably between individuals. Delusions are more common in certain types of dementia, particularly Lewy body dementia, and typically occur more frequently in later stages of the disease. Factors such as the specific brain areas affected, overall health status, and environmental conditions influence whether and when delusions develop.
Key Takeaways
Paranoid delusions are common symptoms in dementia that result from brain changes affecting memory, reasoning, and reality testing. These strongly held false beliefs feel completely real to patients and often involve accusations of theft, harm, or misidentification of family members.
Understanding the neurological basis of delusions helps families respond with greater empathy and effectiveness. Rather than viewing paranoid behaviors as intentional or personal attacks, families can recognize these symptoms as manifestations of brain disease that require patience and specialized management approaches.
Effective management focuses on emotional validation, gentle redirection, and environmental modifications rather than confrontation about the false beliefs. Maintaining calm, supportive relationships while ensuring safety represents the primary goal of delusion management in dementia care.
Professional support becomes essential when delusions significantly impact quality of life, safety, or family relationships. Healthcare providers can offer specialized assessment, treatment recommendations, and ongoing monitoring to help families manage these challenging symptoms effectively.
The most important message for families is that delusions are manageable symptoms that do not reflect the patient’s true feelings about their loved ones. With appropriate understanding, strategies, and support, families can maintain meaningful relationships and provide effective care despite the challenges posed by paranoid thinking in dementia.
References:
[1] Alzheimer’s Society. “Delusions, paranoia and dementia.” February 26, 2021. https://www.alzheimers.org.uk/about-dementia/symptoms-and-diagnosis/delusions