Do you worry that your loved one with dementia knows something is wrong but cannot express it?
Are you concerned about how much they understand about their changing abilities?
These questions keep many families awake at night, wondering whether their family member is suffering in silence or living peacefully unaware of their condition.
Dementia awareness varies significantly depending on the stage of the disease and the individual patient. Research shows that people with dementia may have insight into their condition during early stages, but this awareness typically diminishes as the disease progresses. Understanding this progression can help families provide better support and reduce their own anxiety about their loved one’s experience.
The relationship between dementia and self-awareness is complex and deeply personal. While some patients maintain awareness of their difficulties for extended periods, others may lose this insight relatively early in the disease process. This variation depends on multiple factors, including the type of dementia, the areas of the brain affected, and individual differences in cognitive reserve.
Understanding Awareness in Dementia
Dementia awareness refers to a patient’s ability to recognize and understand their cognitive changes and limitations.
Medical professionals call this insight or disease awareness. This awareness exists on a spectrum rather than being simply present or absent. Some patients may recognize certain difficulties while remaining unaware of others.
The concept of awareness in dementia involves several components. Cognitive awareness relates to understanding memory problems and thinking difficulties. Functional awareness involves recognizing limitations in daily activities. Social awareness encompasses understanding how the condition affects relationships and social interactions.
Research indicates that 60% to 80% of dementia cases involve Alzheimer’s disease, making it the most common form of dementia [1]. The disease affects approximately one-third of people over 85 years of age, though dementia is not a normal part of aging [1]. Understanding how awareness changes in these patients provides crucial insights for families and caregivers.
The brain changes that cause dementia directly impact the areas responsible for self-reflection and insight.
The frontal lobe, which controls executive functions and self-awareness, often experiences damage early in the disease process.
This damage can impair a person’s ability to accurately assess their own cognitive abilities, leading to what researchers call anosognosia – the lack of awareness of one’s own deficits.
| Awareness Component | Early Stage | Middle Stage | Late Stage |
| Memory Problems | Often aware | Variable awareness | Usually unaware |
| Daily Task Difficulties | May recognize | Limited recognition | No recognition |
| Social Changes | Sometimes aware | Rarely aware | Unaware |
| Need for Help | May acknowledge | Often denies | Cannot assess |
What Research Shows About Dementia Awareness
Scientific studies reveal that awareness in dementia follows predictable patterns but varies significantly between individuals. Early-stage patients often maintain some level of insight into their condition, while those in later stages typically lose this awareness entirely.
A comprehensive study published in Medical News Today found that individuals with dementia may experience awareness of their symptoms in the early stages but attribute these changes to normal aging, stress, or anxiety rather than recognizing them as signs of dementia [1]. This misattribution represents a form of partial awareness where patients notice changes but lack understanding of their significance.
The progression of awareness loss correlates strongly with disease severity. Early-stage dementia patients may understand their diagnosis and its implications when explained by healthcare professionals. They can often participate meaningfully in treatment decisions and express preferences about their care. However, as cognitive decline advances, this capacity diminishes progressively.
Research demonstrates that awareness varies by dementia type. Patients with Alzheimer’s disease typically show gradual loss of insight, while those with frontotemporal dementia may lose awareness more rapidly due to early frontal lobe involvement. Lewy body dementia patients often experience fluctuating awareness, with periods of clarity alternating with confusion.
The timing of awareness loss has important implications for families. Studies suggest that patients who maintain awareness longer may experience more distress and anxiety about their condition.
Conversely, those who lose insight earlier may appear more content but require more intensive supervision and care.
The Role of Anosognosia
Anosognosia represents a neurological condition where patients cannot recognize their own deficits. This differs from psychological denial, which involves conscious rejection of uncomfortable truths. In dementia, anosognosia results from brain damage that impairs self-monitoring abilities.
The prevalence of anosognosia in dementia ranges from 20% to 80% depending on the study methodology and patient population examined. This wide range reflects the complexity of measuring awareness and the variability between individuals. Some patients may have anosognosia for specific deficits while maintaining awareness of others.
Understanding anosognosia helps families recognize that their loved one’s lack of insight stems from brain changes rather than stubbornness or denial. This knowledge can reduce frustration and help families develop more effective communication strategies.
Signs and Symptoms to Watch For
Recognizing changes in dementia awareness requires careful observation of how patients respond to their difficulties and limitations. Families should monitor several key indicators that suggest evolving insight into the condition.
Early signs of maintained awareness include patients expressing concern about memory problems, asking questions about their condition, or showing anxiety about their changing abilities. These individuals may actively seek medical attention or request help with tasks they previously managed independently.
Patients with preserved awareness often demonstrate compensatory behaviors. They may write extensive notes, rely heavily on calendars, or ask family members to remind them about important information. These strategies indicate recognition of memory problems and attempts to manage them effectively.
Emotional responses provide important clues about awareness levels. Patients who understand their condition may experience depression, anxiety, or frustration about their limitations.
While these emotions are difficult for families to witness, they often indicate that the person retains insight into their situation.
Conversely, signs of diminishing awareness include patients denying obvious problems, becoming defensive when offered help, or expressing confusion about why family members seem concerned.
These individuals may insist they can drive safely despite clear impairments or claim they never forget anything despite frequent memory lapses.
Language changes also reflect evolving awareness. Patients may stop using words like “forget” or “confused” to describe their experiences. They might attribute difficulties to external factors such as poor lighting, noisy environments, or other people’s mistakes rather than acknowledging their own limitations.
The progression of awareness loss typically follows a predictable pattern. Patients usually lose insight into complex cognitive abilities first, such as judgment and reasoning, while maintaining awareness of basic memory problems longer. Eventually, even awareness of fundamental difficulties disappears.
Communication Patterns and Awareness
Communication changes often signal shifts in dementia awareness. Patients with maintained insight may ask direct questions about their condition, express fears about the future, or discuss their limitations openly. These conversations, while emotionally challenging, indicate preserved self-awareness.
As awareness diminishes, communication patterns change significantly. Patients may avoid discussing their difficulties, change the subject when problems are mentioned, or become agitated when confronted with evidence of their limitations. These responses suggest declining insight into their condition.
Confabulation – creating false memories to fill gaps – often increases as awareness decreases. Patients may provide detailed explanations for their whereabouts or activities that are clearly inaccurate. This behavior typically reflects the brain’s attempt to make sense of incomplete information rather than intentional deception.
Causes and Risk Factors for Awareness Changes
The underlying brain changes in dementia directly impact areas responsible for self-awareness and insight. Understanding these mechanisms helps families appreciate why awareness changes occur and what factors influence the timeline of these changes.
Frontal lobe damage represents the primary cause of awareness loss in dementia. This brain region controls executive functions, including the ability to monitor and evaluate one’s own performance. As dementia progresses, damage to the frontal lobe impairs these self-monitoring capabilities.
The temporal lobe, which processes memory and emotional responses, also plays a crucial role in maintaining awareness. Damage to this region can affect a person’s ability to recognize the significance of memory problems or understand their impact on daily functioning.
Individual factors influence how quickly awareness changes occur. Patients with higher education levels or greater cognitive reserve may maintain insight longer than those with less cognitive resilience. However, this protection is temporary, and awareness eventually diminishes in all patients with progressive dementia.
| Risk Factor | Impact on Awareness | Timeline |
| Frontal Lobe Damage | Rapid awareness loss | Early to middle stage |
| Education Level | Delayed awareness loss | Variable protection |
| Dementia Type | Variable patterns | Depends on type |
| Cognitive Reserve | Extended insight | Individual variation |
| Depression/Anxiety | May preserve awareness | Early stages |
Medication effects can also influence awareness levels. Some medications used to treat dementia symptoms may temporarily improve insight, while others might contribute to confusion or reduced awareness. Regular medication reviews help optimize cognitive function and potentially preserve awareness longer.
Environmental factors play a supporting role in maintaining awareness. Familiar surroundings, consistent routines, and supportive relationships may help patients maintain insight longer than chaotic or stressful environments that overwhelm cognitive resources.
Management and Support Strategies
Supporting patients with varying levels of dementia awareness requires flexible approaches that adapt to changing insight levels. Families and caregivers must balance honesty about the condition with sensitivity to the patient’s emotional well-being and current level of understanding.
For patients with maintained awareness, open communication about the diagnosis and its implications often proves beneficial. These individuals may appreciate honest discussions about their condition, treatment options, and future planning. Providing accurate information helps them maintain autonomy and participate in decision-making while they retain the capacity to do so.
Validation therapy works well for patients who recognize their difficulties. This approach involves acknowledging their concerns, validating their emotions, and providing reassurance about available support. Avoiding dismissive responses like “don’t worry about it” helps maintain trust and emotional connection.
Cognitive stimulation activities may help preserve awareness longer in early-stage patients. Engaging in meaningful activities, maintaining social connections, and continuing familiar hobbies can support cognitive function and potentially extend the period of maintained insight.
For patients with diminishing awareness, different strategies become necessary. Arguing about their limitations or repeatedly correcting their misperceptions typically increases agitation without improving insight. Instead, caregivers should focus on maintaining emotional comfort and safety.
Redirection techniques prove more effective than confrontation for patients with limited awareness. When patients deny problems or become defensive, caregivers can acknowledge their feelings while gently steering conversations toward more positive topics or activities.
Environmental modifications support patients regardless of their awareness level. Creating safe, familiar spaces reduces confusion and anxiety. Clear labeling, consistent routines, and simplified environments help patients function more effectively within their current capabilities.
Communication Strategies by Awareness Level
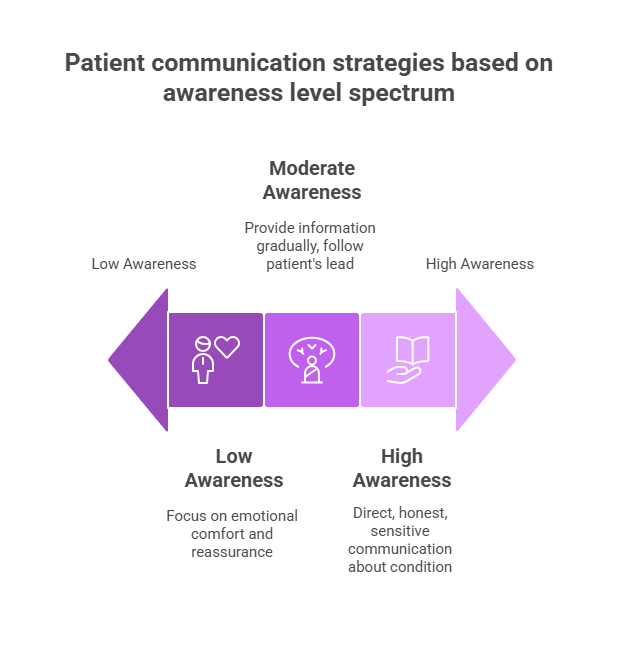
High awareness patients benefit from direct, honest communication delivered with sensitivity and support. These conversations should include information about the condition, available treatments, and resources for support. Patients may want to discuss their fears, make future plans, or express preferences about their care.
Moderate awareness patients require more careful communication approaches. Information should be provided gradually and repeated as needed. These patients may understand some aspects of their condition while remaining unaware of others. Caregivers should follow the patient’s lead in conversations and avoid overwhelming them with too much information at once.
Low awareness patients need communication focused on emotional comfort rather than factual understanding. These individuals may not comprehend explanations about their condition but can still respond to emotional tone and familiar voices. Caregivers should emphasize reassurance, affection, and maintaining dignity.
Practical communication tips include using simple language, speaking slowly and clearly, maintaining eye contact, and allowing extra time for responses. Nonverbal communication becomes increasingly important as verbal abilities decline. Touch, facial expressions, and tone of voice convey meaning even when words lose their impact.
When to Seek Medical Help
Professional evaluation becomes essential when families notice significant changes in their loved one’s awareness or insight into their condition. Healthcare providers can assess cognitive function, adjust treatments, and provide guidance for managing awareness-related challenges.
Immediate medical attention is warranted when patients with previously maintained awareness suddenly lose insight into their condition. This rapid change may indicate delirium, a medical emergency that requires prompt treatment. Delirium can result from infections, medication changes, or other medical conditions that affect brain function.
Signs requiring medical evaluation include sudden confusion, dramatic personality changes, new behavioral problems, or significant decline in daily functioning. These changes may indicate treatable conditions that are affecting cognitive function and awareness levels.
Regular medical monitoring helps track awareness changes over time and adjust care plans accordingly. Healthcare providers can assess whether awareness loss follows expected patterns or suggests other medical issues requiring attention.
Questions to ask healthcare providers include inquiries about the expected timeline for awareness changes, strategies for supporting patients at different awareness levels, and available resources for families dealing with these challenges.
| Symptom | Urgency Level | Recommended Action |
| Sudden awareness loss | High | Immediate medical evaluation |
| Gradual awareness decline | Moderate | Schedule routine appointment |
| Increased agitation about condition | Moderate | Discuss with healthcare team |
| New behavioral problems | High | Prompt medical assessment |
| Medication side effects | High | Contact prescribing physician |
Support services can help families navigate awareness-related challenges. Social workers, counselors, and support groups provide valuable resources for understanding and managing these difficult situations. Many communities offer specialized programs for families dealing with dementia-related awareness issues.
Frequently Asked Questions
Do people with dementia know they are confused?
In the early stages of dementia, patients may be aware of their confusion but often attribute these symptoms to anxiety, stress, or normal aging rather than recognizing them as signs of dementia. As the condition progresses, individuals typically lose the ability to recognize or communicate their confusion effectively. The awareness of confusion varies significantly between patients and changes over time as the disease advances.
Can dementia patients understand what you are saying to them?
Understanding in dementia patients varies considerably depending on the stage of the disease and the complexity of the communication. Early-stage patients typically understand most conversations, while those in later stages may comprehend emotional tone and simple phrases even when complex language becomes difficult to process. Patients often retain the ability to understand more than they can express, making clear, simple communication important throughout the disease progression.
How long do dementia patients maintain awareness of their condition?
The duration of maintained awareness varies widely between individuals and depends on factors such as the type of dementia, rate of progression, and individual cognitive reserve. Some patients may maintain partial awareness for several years, while others lose insight relatively quickly. Most patients experience gradual awareness loss over months to years rather than sudden complete loss of insight.
Should you tell someone with dementia they have dementia?
Disclosure decisions should be individualized based on the patient’s current awareness level, emotional stability, and expressed desire for information. Patients with maintained awareness often benefit from honest, supportive discussions about their condition. However, repeatedly reminding patients with limited awareness about their diagnosis may cause unnecessary distress without providing benefit. Healthcare providers can help families determine the most appropriate approach for each situation.
What is the difference between denial and lack of awareness in dementia?
Denial represents a psychological defense mechanism where patients consciously reject uncomfortable truths about their condition. Lack of awareness (anosognosia) results from brain damage that impairs the ability to recognize deficits. Patients in denial may acknowledge problems when presented with evidence, while those with anosognosia cannot recognize their limitations even when confronted with clear evidence. Understanding this distinction helps families respond more effectively to their loved one’s reactions.
Key Takeaways
Dementia awareness exists on a spectrum and changes predictably as the disease progresses. Early-stage patients often maintain some insight into their condition, while those in later stages typically lose this awareness due to brain changes affecting self-monitoring abilities. Understanding these patterns helps families provide appropriate support and reduces anxiety about their loved one’s experience.
Individual variation in awareness patterns means that each patient’s journey will be unique. Factors such as education level, cognitive reserve, and dementia type influence how quickly awareness changes occur. Families should focus on adapting their communication and support strategies to match their loved one’s current level of insight rather than expecting consistent awareness throughout the disease progression.
Professional support proves invaluable for families navigating awareness-related challenges. Healthcare providers can assess cognitive function, provide guidance for communication strategies, and help families understand what to expect as the disease progresses. Regular medical monitoring ensures that awareness changes follow expected patterns and helps identify any treatable conditions that might be affecting cognitive function.
The most important message for families is that lack of awareness does not mean lack of feeling. Even patients who cannot recognize their limitations still experience emotions and respond to love, comfort, and familiar voices. Focusing on emotional connection and maintaining dignity provides meaningful support regardless of awareness level.
References:
[1] Medical News Today. “Does someone with dementia know they have it?” Updated January 9, 2024. https://www.medicalnewstoday.com/articles/do-people-with-dementia-know-they-have-it