Does your loved one with dementia resist bathing or become agitated around water? Do they seem frightened when you try to help them shower or wash their hands? Are you struggling to maintain their hygiene because they appear terrified of water that once brought them comfort? These water-related fears are more common than many families realize.
Water fear in dementia patients stems from changes in visual perception, sensory processing, and cognitive understanding that make water seem threatening or confusing. What appears as simple aquaphobia often involves complex neurological changes that affect how patients see, feel, and interpret water-related experiences.
Understanding why dementia patients develop fear of water helps families approach hygiene care with greater patience and develop strategies that reduce anxiety while maintaining cleanliness and dignity. These fears are not stubbornness or behavioral problems but represent genuine neurological symptoms that require specialized approaches.
Why Dementia Patients Develop Water Fears
Multiple neurological changes work together to create water fears in dementia patients. Understanding these underlying causes helps families recognize that water fears represent genuine symptoms rather than behavioral problems.
Visual and Sensory Changes
Visual perception problems make water particularly challenging for dementia patients. Since water is transparent, patients with dementia-related vision changes cannot see it clearly. Water may appear completely invisible, making contact unexpected and frightening. This transparency issue affects both drinking and bathing activities.
Sensory processing alterations dramatically change how water feels against the skin. Many dementia patients describe shower water as feeling like insects crawling on their skin or other unpleasant sensations. These altered nerve responses create genuine physical discomfort that patients naturally want to avoid.
Temperature sensitivity increases significantly in dementia patients due to both aging skin and dementia-related changes. Water that feels comfortable to caregivers may feel burning hot or freezing cold to patients, creating additional barriers to water activities.
Cognitive and Emotional Factors
Memory and recognition deficits prevent patients from understanding water’s purpose and safety. Without memory connections to positive bathing experiences or understanding of hygiene needs, water contact seems pointless and threatening. Patients may not recognize water as a familiar substance.
Loss of control represents a major factor in water fears. Patients who once managed their own hygiene independently feel vulnerable and frightened when they need help with intimate care activities. This loss of autonomy creates anxiety that becomes associated with water itself.
Past traumatic experiences with water may become more significant in dementia patients who lose the ability to distinguish between past and present. Previous water-related trauma may feel immediate and current to patients with memory problems.
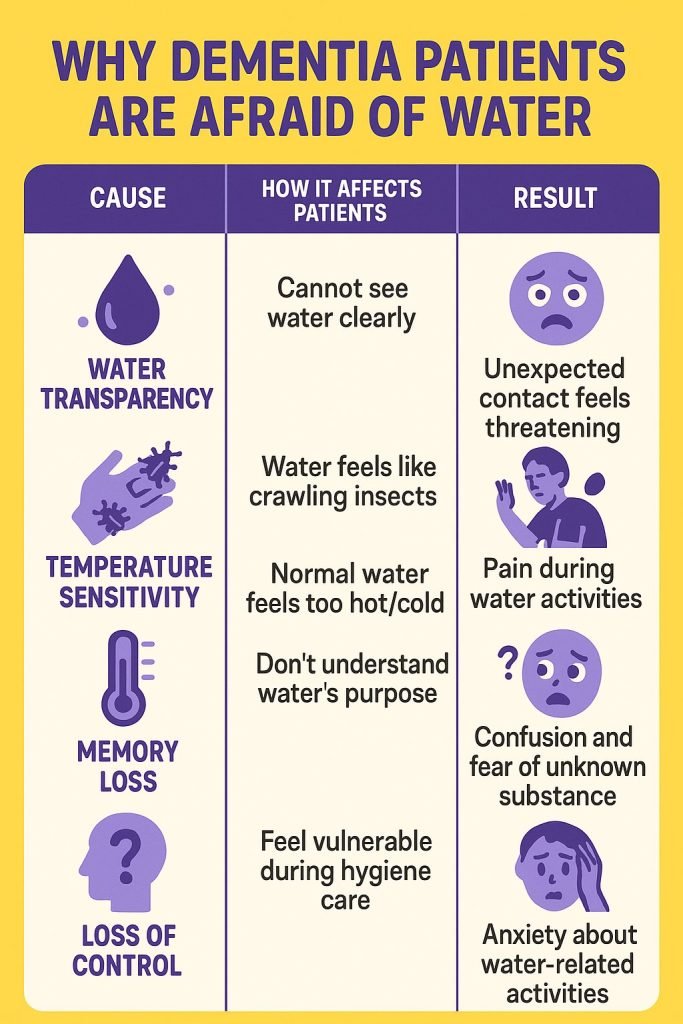
| Cause | How It Affects Patients | Result |
| Water transparency | Cannot see water clearly | Unexpected contact feels threatening |
| Altered sensations | Water feels like crawling insects | Physical discomfort and avoidance |
| Temperature sensitivity | Normal water feels too hot/cold | Pain during water activities |
| Memory loss | Don’t understand water’s purpose | Confusion and fear of unknown substance |
| Loss of control | Feel vulnerable during hygiene care | Anxiety about water-related activities |
Research Findings on Water Fears
Research from Home Care Assistance demonstrates that seniors with dementia sometimes develop aquaphobia as part of their condition, with multiple underlying causes contributing to these water-related fears. Studies reveal specific patterns that help explain why these fears develop.
Visual perception research shows that dementia patients often cannot see water clearly due to transparency issues. This invisible water problem makes it difficult for patients to understand what they are interacting with. Research suggests that tinting water with colored juice can make it more visible and less threatening for drinking purposes.
Sensory studies demonstrate that dementia significantly alters water sensation experiences. The heightened sensory input associated with dementia makes normal water pressure feel overwhelming or painful. Studies indicate that low-pressure settings and bath alternatives can reduce sensory distress.
Bathing research reveals that water fears often relate to broader issues around privacy, dignity, and loss of control rather than fear of water itself. Many patients who appear afraid of water are actually responding to vulnerability and embarrassment associated with needing help with intimate care.
Brain imaging studies show that dementia affects multiple areas involved in sensory processing. The parietal lobe (sensory processing) and temporal lobe (memory and recognition) both show changes that affect water perception and understanding.
Recognizing Water Fear Signs
Direct water responses include obvious distress when water is present. Patients may scream, pull away, or become combative when water touches their skin. Physical signs include tension, rapid breathing, or attempts to escape from water situations.
Avoidance behaviors develop as patients learn to anticipate water activities. They may resist going to bathrooms, refuse to approach sinks, or become agitated when they see bathing supplies. Some patients hide when they know bath time approaches.
Communication changes provide important clues about developing fears. Patients may use words like “scary,” “hurts,” or “don’t like” when water is mentioned. They may develop their own terms for describing uncomfortable water sensations.
Hygiene decline often results from water fears. Families notice resistance to tooth brushing, hand washing, and face cleaning in addition to bathing resistance. This decline can lead to health problems if not addressed promptly.
Sleep disturbances may occur if patients become anxious about upcoming water activities. Some have difficulty sleeping before scheduled bath days or become agitated when anticipating hygiene care.
Behavioral Patterns to Monitor
Escalation patterns often develop around water activities, with distress increasing as water contact approaches. Understanding these patterns helps caregivers intervene earlier to reduce anxiety.
Timing sensitivity affects patient responses to water activities. Some patients are more receptive at certain times when they are calmer or more alert. Identifying optimal timing significantly improves water care experiences.
Environmental triggers may worsen water fears. Bright lights, loud noises, cold temperatures, or unfamiliar people compound water-related anxiety. Creating calm environments helps reduce overall stress.
Effective Management Strategies
Comprehensive approaches to managing water fears involve environmental modifications, communication strategies, and alternative hygiene methods that prioritize patient comfort while maintaining cleanliness and health.
Environmental and Technical Solutions
Environmental modifications create more comfortable water experiences:
•Improve lighting to help patients see water more clearly
•Reduce noise and maintain warm temperatures for comfort
•Use non-slip mats and grab bars for safety
•Create calm, familiar environments during water activities
Water pressure adjustments reduce sensory overwhelm:
•Use low-flow showerheads with gentle spray settings
•Pour water slowly rather than using direct shower streams
•Consider warm washcloths instead of flowing water
•Test different pressure levels to find patient comfort zones
Temperature management requires careful attention:
•Test water temperature with thermometers
•Adjust based on patient responses rather than standard recommendations
•Some patients prefer slightly warmer or cooler water
•Monitor for signs of discomfort throughout activities
Alternative Hygiene Approaches
Water alternatives provide effective cleaning while reducing anxiety:
•No-rinse cleansing products for body cleaning
•Dry shampoos for hair care
•Warm washcloth baths instead of showers
•Partial bathing that cleans one area at a time
Gradual exposure techniques help patients become more comfortable over time:
•Start with small amounts of water like damp cloths
•Gradually increase water contact as tolerance improves
•Proceed at the patient’s pace and stop if distress increases
•Celebrate small successes to build positive associations
Communication and Support Strategies
Communication approaches focus on reassurance and simple explanations:
•Use calm tones and simple language
•Explain each step of water activities
•Use familiar terms the patient understands
•Provide constant reassurance throughout the process
Timing optimization involves identifying the best times for water care:
•Some patients are more cooperative in mornings, others prefer evenings
•Avoid times when patients are tired, hungry, or agitated
•Allow extra time to reduce rushing and pressure
•Be flexible with scheduling based on patient needs
Distraction methods redirect attention away from water fears:
•Play familiar music during hygiene activities
•Engage in conversation about pleasant topics
•Provide something to hold like a washcloth or toy
•Use aromatherapy or other pleasant sensory experiences
| Strategy Type | Specific Techniques | Expected Outcome |
| Environmental | Improved lighting, reduced noise | Better water visibility, less anxiety |
| Technical | Low-pressure water, temperature control | Reduced sensory overwhelm |
| Alternative methods | No-rinse products, washcloth baths | Maintained hygiene without water fears |
| Communication | Simple explanations, reassurance | Reduced confusion and anxiety |
| Timing | Optimal scheduling, flexibility | Better cooperation and success |
When to Seek Professional Help
Medical evaluation becomes important when water fears significantly interfere with hygiene maintenance or when patients show signs of dehydration from drinking avoidance. Healthcare providers can assess underlying causes and recommend interventions.
Immediate medical attention is required for:
•Dangerous dehydration from drinking avoidance
•Serious hygiene-related health problems like infections
•Extreme agitation that poses safety risks
•Sudden onset of severe water fears
Specialist consultations with occupational therapists, geriatricians, or dementia specialists can provide additional strategies. These professionals offer specialized techniques and equipment recommendations that improve water-related care.
Medication reviews may help if water fears develop suddenly or worsen significantly. Some medications affect sensory perception or increase anxiety, contributing to water-related fears.
| Concern Level | Symptoms | Recommended Action |
| High Priority | Dehydration, infections, extreme agitation | Immediate medical evaluation |
| Moderate Priority | Sudden onset fears, medication effects | Schedule medical appointment |
| Ongoing Monitoring | Gradual worsening, hygiene decline | Regular healthcare provider communication |
Frequently Asked Questions
Why do dementia patients suddenly become afraid of water?
Water fears develop due to brain changes affecting visual perception, sensory processing, and cognitive understanding. Dementia makes water appear invisible, feel unpleasant, or seem threatening due to loss of understanding about its purpose. These represent neurological symptoms, not behavioral problems.
How can families help dementia patients who are afraid of water?
Help involves creating comfortable environments, using gentle approaches, and considering alternatives to traditional water contact. Key strategies include improving lighting, reducing water pressure, maintaining appropriate temperatures, using washcloths instead of showers, and providing constant reassurance.
Are there alternatives to traditional bathing?
Yes, alternatives include no-rinse cleansing products, warm washcloth baths, dry shampoos, and partial bathing approaches. These maintain cleanliness while reducing water-related anxiety. Professional hygiene services specializing in dementia care are also available.
Can water fears be overcome?
Water fears can often be managed effectively through gradual exposure, environmental modifications, and alternative approaches. Complete elimination may not always be possible, but significant improvement in water-related anxiety is achievable with appropriate strategies.
When should families be concerned about water fears?
Concerning situations include severe dehydration from drinking avoidance, significant hygiene decline leading to health problems, extreme agitation during water activities, or sudden onset of severe fears. These situations require medical evaluation and professional intervention.
Key Takeaways
Water fears in dementia patients result from complex neurological changes affecting how they see, feel, and understand water. These fears are genuine symptoms requiring patience, understanding, and specialized management approaches rather than confrontation.
Effective management combines environmental modifications, alternative hygiene approaches, and communication strategies that prioritize patient comfort and dignity. Success requires flexibility, creativity, and willingness to adapt traditional routines to individual needs.
Professional support provides valuable assistance for families struggling with water-related care challenges. Healthcare providers and specialists offer techniques and recommendations that improve outcomes for both patients and caregivers.
The most important message for families is that water fears are manageable with appropriate understanding and strategies. While challenging, maintaining patience and focusing on patient comfort helps preserve dignity while ensuring necessary hygiene care throughout the dementia journey.