Are you concerned that your loved one with dementia might be suffering in silence?
Do you wonder if their behavioral changes or agitation could be signs of untreated pain?
Are you struggling to understand whether they can communicate their discomfort effectively?
These concerns weigh heavily on families caring for someone with dementia.
Pain in dementia patients is far more common than many people realize, with research showing that 50% to 80% of patients with moderate to severe dementia experience pain daily.
Unfortunately, many of these patients receive inadequate treatment due to difficulties in recognizing and assessing pain in individuals with cognitive impairment.
Understanding how dementia affects pain perception and expression helps families and caregivers provide better support and advocate for appropriate pain management.
Pain assessment in dementia requires special approaches since traditional methods like asking patients to rate their pain on a scale become ineffective as cognitive abilities decline.
Understanding Pain in Dementia
Pain perception in dementia patients involves complex interactions between physical sensations, cognitive processing, and communication abilities. While the basic ability to feel pain typically remains intact throughout most stages of dementia, the capacity to recognize, interpret, and communicate pain experiences becomes increasingly impaired.
Dementia affects pain in multiple ways that create significant challenges for patients, families, and healthcare providers. The disease impacts brain regions responsible for processing pain signals, interpreting their meaning, and formulating appropriate responses. This neurological damage can alter how patients experience and express pain.
The prevalence of pain in dementia is staggering. Research from Mayo Clinic Health System indicates that between 50% and 80% of patients with moderate to severe dementia experience pain daily [1]. This high prevalence reflects both the increased likelihood of painful conditions in older adults and the challenges of managing pain in cognitively impaired individuals.
Chronic pain affects the same brain areas that are impacted by Alzheimer’s disease, creating a complex relationship between pain and cognitive decline. The locus coeruleus brain region and the chemical messenger norepinephrine play crucial roles in both pain processing and dementia progression. As norepinephrine is released, it can cause pain-relaying cells in the brain to become inflamed, potentially worsening both pain and cognitive symptoms.
The degree of cognitive decline in patients with Alzheimer’s disease can be directly correlated with the severity of pain experienced. This means that patients without other apparent causes of pain could still be experiencing significant discomfort due to neuroinflammation in the brain caused by the disease process itself.
| Pain Type | Prevalence in Dementia | Recognition Challenges | Management Approach |
|---|---|---|---|
| Chronic pain | 50-80% of moderate-severe cases | Reduced verbal expression | Behavioral observation |
| Acute pain | Variable | Mask-like facial expressions | Physical examination |
| Neuropathic pain | Common | Difficulty describing sensations | Specialized medications |
| Inflammatory pain | Frequent | Limited awareness of symptoms | Anti-inflammatory treatments |
What Research Shows About Pain in Dementia

Scientific studies reveal that pain in dementia presents unique challenges that require specialized understanding and approaches. Research published by Mayo Clinic Health System demonstrates that pain is often overlooked and undertreated in dementia patients, leading to unnecessary suffering and complications [1].
Alzheimer’s disease causes patients to develop a mask-like facial expression that minimizes typical pain expressions such as drawn mouth or furrowed brows. This neurological change makes it extremely difficult for caregivers and healthcare providers to recognize pain through traditional visual cues that would normally indicate discomfort.
The loss of cognitive ability to communicate pain represents one of the most significant challenges in dementia care. Patients may lose the capacity to tell caregivers about their pain using phrases such as “this hurts” or “I am in pain.” This communication barrier leaves many patients unable to advocate for their own comfort and pain relief.
Behavioral expressions become the primary way dementia patients communicate pain when verbal abilities decline. Unfortunately, these expressions often manifest as negative behaviors including screaming, cursing, or striking out, particularly directed at caregivers. These behaviors are frequently misinterpreted as aggression or behavioral problems rather than recognized as pain communication.
Untreated pain creates a cascade of additional problems for dementia patients. Pain can cause patients to become more withdrawn or fatigued, either due to their discomfort or lack of restorative sleep. Even though patients may appear drowsy and sleep more than before, their sleep becomes disturbed and non-restorative when pain is present.
The Pain-Dementia Connection
Neuroinflammation represents a key mechanism linking chronic pain and Alzheimer’s disease. The brain changes that occur in dementia can intensify pain processing, making patients more sensitive to painful stimuli even when the original source of pain is relatively minor.
Pain assessment challenges in dementia stem from the progressive loss of language abilities and self-awareness. Traditional pain assessment tools that rely on patient self-report become ineffective as cognitive decline advances. This creates a significant gap in pain management that requires alternative assessment approaches.
Research findings indicate that patients with dementia who experience pain show marked increases in caregiver stress. This creates a difficult cycle where untreated pain in patients leads to increased burden on caregivers, potentially affecting the quality of care provided.
The Pain Assessment in Advanced Dementia Scale (PAINAD) was developed specifically to address the challenges of assessing pain in cognitively impaired patients. This tool evaluates five behavioral indicators: breathing, negative vocalization, facial expression, body language, and consolability. The scale can be used by people without medical training and does not require language skills from the patient.
Signs and Symptoms to Watch For
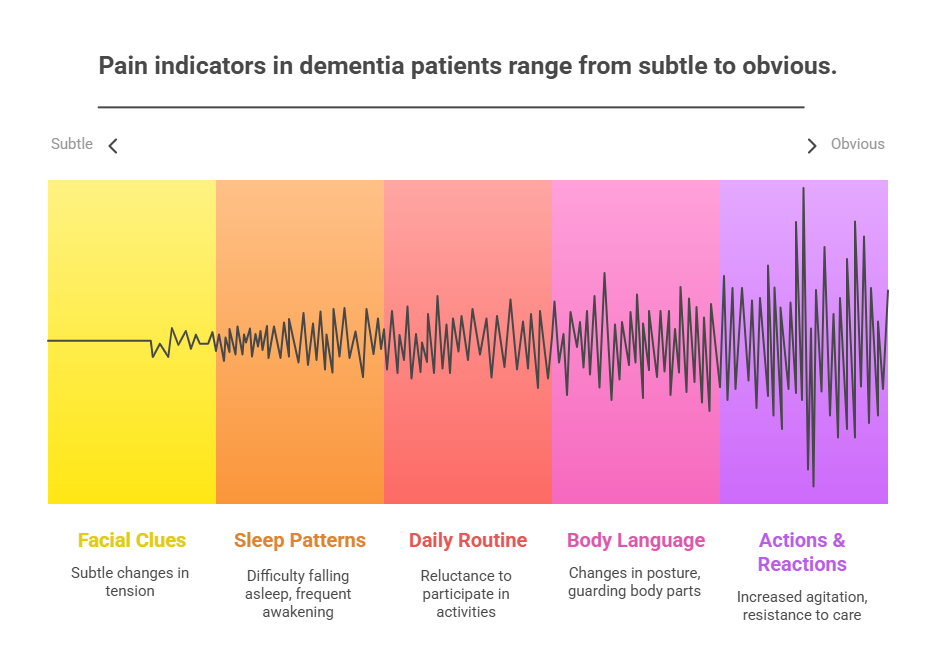
Recognizing pain in dementia patients requires careful observation of behavioral changes, physical signs, and alterations in daily functioning patterns. Since verbal communication becomes limited, caregivers must become skilled at interpreting non-verbal pain indicators.
Physical signs of pain may include changes in posture, guarding of specific body parts, reluctance to move or be touched, and alterations in sleep patterns. Patients may also show changes in appetite, increased restlessness, or unusual positioning that suggests they are trying to find comfort.
Behavioral indicators often provide the clearest evidence of pain in dementia patients. These may include increased agitation, resistance to care activities, crying or moaning, aggressive behaviors, or withdrawal from social interactions. Some patients may exhibit repetitive movements or vocalizations that suggest discomfort.
Facial expressions can provide valuable clues about pain, even when the typical pain expressions are diminished. Caregivers should watch for subtle changes in facial tension, eye closure, or grimacing that may indicate discomfort. Some patients may show pain through rapid blinking, clenched jaw, or other facial muscle tension.
Changes in daily activities often signal the presence of pain. Patients may become reluctant to participate in activities they previously enjoyed, show resistance to personal care tasks, or demonstrate decreased mobility. These changes may be gradual and easily attributed to disease progression rather than recognized as pain indicators.
Sleep disturbances frequently accompany pain in dementia patients. Patients may have difficulty falling asleep, experience frequent awakening, or show increased confusion and agitation during nighttime hours. Poor sleep quality can worsen both pain and cognitive symptoms, creating a challenging cycle.
Specific Pain Behaviors
Vocalization patterns can indicate pain even when patients cannot articulate their discomfort clearly. Moaning, groaning, calling out, or repetitive vocalizations may signal pain, especially if these behaviors represent changes from the patient’s baseline communication patterns.
Movement changes provide important clues about pain location and severity. Patients may favor one side of their body, avoid certain movements, or show stiffness that suggests musculoskeletal pain. Some patients may exhibit restlessness or inability to find comfortable positions.
Interaction changes with caregivers and family members often reflect pain status. Patients experiencing pain may become more irritable, less cooperative with care activities, or show increased resistance to touch or movement. These changes may be particularly noticeable during personal care tasks.
Causes and Risk Factors for Pain in Dementia
Multiple factors contribute to the high prevalence of pain in dementia patients. Understanding these causes helps caregivers and healthcare providers develop comprehensive pain management strategies that address both the underlying conditions and the unique challenges of dementia care.
Previous injuries and surgeries often become sources of chronic pain as patients age and become less mobile. Conditions such as old knee or hip replacements, previous fractures, or tennis elbow injuries can become painful when patients become less active. Joint stiffness develops when joints are not used regularly, leading to discomfort and reduced mobility.
Contractures represent a significant source of pain in advanced dementia patients. These occur when muscles, skin, tendons, and tissues tighten due to prolonged immobility or positioning. Patients may avoid being repositioned or using painful body parts, which contributes to the development of these painful conditions.
Pressure ulcers can develop when patients spend significant time in the same position, leading to skin breakdown and pain. These wounds are particularly problematic because patients may not be able to communicate their discomfort or request position changes to relieve pressure.
Underlying medical conditions such as cancer, heart disease, or kidney disease can cause pain that becomes more difficult to assess and treat in dementia patients. Caregivers may not realize these conditions have worsened because patients cannot verbally express symptoms like chest pain or flank pain.
| Pain Source | Prevalence | Recognition Difficulty | Management Strategy |
|---|---|---|---|
| Musculoskeletal conditions | Very high | Moderate | Physical therapy, positioning |
| Previous injuries | High | High | Medication, gentle movement |
| Pressure ulcers | Moderate | Low | Prevention, wound care |
| Internal medical conditions | Variable | Very high | Regular medical monitoring |
| Dental problems | High | High | Regular dental examinations |
Mental and emotional pain can be exacerbated by dementia, even when patients are confused or disoriented. Patients may experience significant loss or grief that manifests as physical pain. This social, spiritual, or emotional pain is felt physically like other types of pain and requires recognition and appropriate support.
Medication-related pain can occur from side effects of dementia medications or interactions between multiple drugs. Some medications may cause muscle pain, headaches, or gastrointestinal discomfort that patients cannot effectively communicate.
Management and Support Strategies
Comprehensive pain management in dementia requires a multimodal approach that combines medication and non-medication interventions. The goal is to provide effective pain relief while minimizing side effects and maintaining the patient’s quality of life and functional abilities.
Medication management follows the principle of using the lowest effective dose to achieve pain relief. Healthcare teams work to identify the specific type of pain patients are experiencing to select the most appropriate medications. Neuropathic pain that burns, tingles, or travels requires medications specific to the nervous system, while inflammatory pain responds better to anti-inflammatory drugs.
Multimodal pain therapy involves using several medications together, each with a specific role in pain management. This approach allows for lower doses of individual medications while achieving better overall pain control. For example, cancer pain may require multiple medications working together to address different aspects of the pain experience.
Non-medication treatments often provide significant pain relief without the side effects associated with drugs. These approaches can be particularly valuable for dementia patients who may be sensitive to medication effects or already taking multiple drugs for other conditions.
Massage therapy can provide effective pain relief and does not require specialized training for caregivers to implement. Simple techniques such as gentle massage of swollen or stiff joints can provide comfort. Caregivers should watch for relaxed body position, improved facial expressions, and slower breathing as indicators that massage is helpful.
Music therapy offers a beautiful approach to pain management that can be easily implemented by families. Playing music that patients enjoyed in their youth can help distract from pain and release natural endorphins that reduce discomfort. Music can also help orient patients and bring pleasant feelings and memories that counteract pain experiences.
Practical Pain Management Techniques
Positioning strategies play a crucial role in pain management for dementia patients. Regular position changes help prevent pressure ulcers and reduce stiffness. Caregivers should watch for relaxed facial expressions and body language to ensure new positions provide comfort rather than increased discomfort.
Environmental modifications can significantly impact pain levels. Ensuring comfortable room temperature, appropriate lighting, and reducing noise levels helps create a soothing environment that supports pain management. Some patients may benefit from soft music, aromatherapy, or other sensory interventions.
Activity modifications help balance the need for movement with pain management goals. Gentle exercises, range of motion activities, and participation in enjoyable activities can help manage pain while maintaining function. The key is finding the right balance for each individual patient.
Heat and cold therapy can provide pain relief for specific conditions. Warm compresses may help with muscle stiffness, while cold packs can reduce inflammation. Caregivers should use these therapies carefully and monitor skin condition to prevent injury.
When to Seek Medical Help
Immediate medical attention is required when dementia patients show signs of severe pain that cannot be managed with current interventions. Signs requiring urgent evaluation include sudden onset of severe agitation, new behavioral problems that suggest pain, or physical signs such as swelling, redness, or obvious injury.
Regular pain assessments should be conducted by healthcare providers to ensure optimal pain management. These evaluations should include review of current medications, assessment of pain behaviors, and consideration of new or worsening medical conditions that might be causing pain.
Medication reviews are essential for dementia patients receiving pain medications. Healthcare providers need to monitor for side effects, drug interactions, and effectiveness of current pain management strategies. Some pain medications can worsen confusion or increase fall risk in dementia patients.
Signs requiring medical evaluation include changes in pain behaviors, new or worsening agitation, sleep disturbances, decreased appetite, or resistance to care activities that were previously tolerated. These changes may indicate inadequate pain control or new medical problems requiring attention.
| Symptom | Urgency Level | Recommended Action |
|---|---|---|
| Sudden severe agitation | High | Immediate medical evaluation |
| New resistance to care | Moderate | Schedule medical appointment |
| Changes in sleep/appetite | Moderate | Discuss with healthcare provider |
| Obvious physical injury | High | Seek immediate medical attention |
| Medication side effects | High | Contact prescribing physician |
Specialist consultations may be beneficial for complex pain management situations. Pain specialists, geriatricians, or palliative care physicians can provide expertise in managing pain in dementia patients while considering the unique challenges these patients face.
Frequently Asked Questions
How can you tell if someone with dementia is in pain?
Recognizing pain in dementia patients requires careful observation of behavioral changes, facial expressions, and alterations in daily functioning. Key indicators include increased agitation, resistance to care, changes in sleep patterns, decreased appetite, and unusual vocalizations. The PAINAD scale provides a structured approach to pain assessment that evaluates breathing, vocalization, facial expression, body language, and consolability.
Can dementia patients feel pain the same way as others?
Pain sensation typically remains intact in dementia patients, but their ability to recognize, interpret, and communicate pain becomes impaired. The neuroinflammation associated with dementia may actually intensify pain processing, making patients more sensitive to painful stimuli. However, their reduced ability to express pain verbally means they often suffer in silence.
What types of pain are most common in dementia patients?
Common pain types include musculoskeletal pain from arthritis or old injuries, pain from pressure ulcers or contractures, dental pain, and pain from underlying medical conditions. Chronic pain is particularly prevalent, affecting the same brain areas involved in dementia progression. Many patients also experience pain directly related to the neuroinflammation caused by the dementia disease process.
Are pain medications safe for dementia patients?
Pain medications can be safe and effective for dementia patients when used appropriately and monitored carefully. The key is using the lowest effective dose and choosing medications that minimize cognitive side effects. Healthcare providers must balance pain relief with the risk of increased confusion, falls, or other complications. Non-medication approaches should be used whenever possible to supplement or reduce medication needs.
How does untreated pain affect dementia patients?
Untreated pain can significantly worsen dementia symptoms, leading to increased confusion, agitation, and behavioral problems. Pain can disrupt sleep, reduce appetite, and decrease participation in activities, all of which can accelerate cognitive decline. Patients with untreated pain may become more withdrawn, experience depression, and have reduced quality of life. Additionally, untreated pain increases caregiver stress and burden.
Key Takeaways
Pain is extremely common in dementia patients, with 50-80% of those with moderate to severe dementia experiencing daily pain. Unfortunately, this pain is often unrecognized and undertreated due to communication barriers and changes in pain expression that occur with cognitive decline.
Recognition requires specialized approaches since traditional pain assessment methods become ineffective as dementia progresses. Caregivers must learn to interpret behavioral changes, facial expressions, and alterations in daily functioning as potential indicators of pain. The PAINAD scale provides a valuable tool for systematic pain assessment in non-verbal patients.
Comprehensive management involves both medication and non-medication approaches tailored to the individual patient’s needs and capabilities. Effective pain management can significantly improve quality of life, reduce behavioral problems, and decrease caregiver stress. Regular medical monitoring ensures optimal pain control while minimizing side effects.
Family advocacy plays a crucial role in ensuring adequate pain management for dementia patients. Caregivers who understand pain indicators and communicate effectively with healthcare providers can help ensure their loved ones receive appropriate pain relief and maintain comfort throughout their dementia journey.
The most important message for families is that pain in dementia is treatable. While the challenges are significant, understanding pain indicators and working with healthcare providers to develop comprehensive management strategies can provide meaningful relief and improve quality of life for both patients and their caregivers.
References:
[1] Mayo Clinic Health System. “Dementia-related pain management.” January 26, 2023. https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/dementia-related-pain-and-caregivers